Need a Headline Here
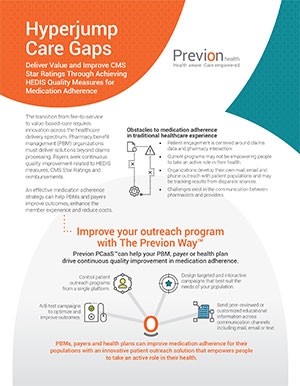
The transition from fee-to-service to value-based-care requires innovation across the healthcare delivery spectrum. Pharmacy benefit management (PBM) organizations must deliver solutions beyond claims processing. Payers seek continuous quality improvement related to HEDIS measures, CMS Star Ratings and reimbursements.
Pharmacies and healthcare providers play an active role in education and communication with their populations to help empower people to take action.
An effective medication adherence strategy can help enhance the member experience and reduce costs.